
Treatment

What happens at your first appointment?
The initial visit to a podiatrist normally lasts 20-30 minutes during which time a full assessment of your foot condition will be made. Your treatment options will be discussed in full and an appropriate treatment will be recommended and discussed. In most cases treatment will be started during your first visit.
Foot Surgery
Where appropriate Anna may offer you advise on foot surgery to help resolve your pain or problem. Anna gives Surgical consultations and advise on:
Conditions We Treat
Is it time to visit Complete Foot Care at the Balcombe Foot and Ankle Clinic?
Yes, if you are suffering from any of the below. Please click on each to find out more.
Achilles tendonitis develops due to inflammation, strain, or repetitive trauma to the Achilles tendon at the back of the heel. This occurs usually due to a repetitive activity. Symptoms are often brought on by sports such as running, tennis and basketball.
If left untreated, it can develop into Achilles tendinitis, where there is a degenerative change in the tendon from repetitive micro-trauma. The tendon scars and the injury become a long term problem.
Complete Foot Care at the Balcombe Foot and Ankle Clinic can provide treatment and advise to resolve Achilles tendonitis through advice, strapping, massage, rehabilitation and orthotics where necessary.
There are a variety of conditions that affect the ankle and cause patients ankle pain.
What are these and how can The Balcombe Foot and Ankle Clinic help?
Ankle sprains arise from poor foot mechanics, running/ walking on uneven surfaces, previous ankle injury and poor rehabilitation plus inadequate footwear. Repetitive stress and a build up of scar tissue can cause ankle pain. Treatment will include addressing all the factors above.
Posterior tibial tendonitis gives a pain with weight bearing that can extend from the mid calf, behind the inside of the ankle joint and into the arch of the foot. The posterior tibial tendon becomes swollen and painful especially on tip toe. Physical therapies, massage, orthotics and Podiatric advice can treat this successfully.
Ankle Capsule Impingement is where the joint capsule of the ankle is pinched at the front of the ankle causing ankle pain with exercise.
Peroneal Tendonitis occurs with overuse of the tendon running across the top and outside of the foot and ankle. It is painful with exercise, walking and when patients are on tip toe or walking up stairs.
Retro calcaneal bursitis is a swelling of the fluid filled sac that sits at the back of the heel bone, deep to the Achilles. The Achilles tendon itself isn’t painful but the deeper structures are tender to touch.

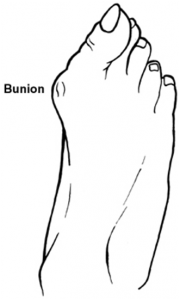
What is a bunion?
When your big toe is angled towards the second toe, the deformity is called a bunion (hallux valgus). This causes a bump on the side at the base of the big toe. There can also be thickening of the skin and tissues of the joint which can be become inflamed, swollen and painful. Due to this deformity the bones of the big toe are pushed towards the smaller toes and can displace them and can cause hammer (bent into an inverted “V” position) toes.
What are symptoms of hammer toes?
- Pain at the top of the bent toe when putting on a shoe.
- Corns forming on the top of the toe joint.
- The toe joint swelling and becoming red and inflamed.
- Difficulty in moving the toe joint – and pain when you try to.
- Pain on the ball of the foot under the bent toe.
Treatment for bunions and hammer toes may include:
- Footwear advice, trainers or slippers that fit well and are roomy and to avoid tight high heeled shoes.
- Padding over the bunion , toes
- Ice packs
- Anti-inflammatory gels and medicines
- Ultrasound and physical therapies
- Strapping
- Orthotics
- Devices which help to straighten the toe ( toe braces and toe props)
- Surgical correction
What is a bursitis?
A bursa is a small fluid filled sac that forms in areas of extra rubbing and friction. When this bursa or sac like structure becomes swollen and inflamed due to abnormally high pressure through the tissue, it is called bursitis.
Symptoms of bursitis usually occur after rest and relaxation. With activity the pain increases in the area of the bursa. Common areas to have a bursitis in the foot are in the bottom of the heel, behind the heel near the attachment of the Achilles tendon as well as along the side of a bunion.
A bursa may also form in multiple areas especially along the metatarsal heads, or “ball” of your foot. It may actually feel the sac like fluid when rubbing the area of pain.
How do I Treat Bursitis?
With good Podiatric Care at The Balcombe Foot and Ankle Clinic.
Treatment may include using anti-inflammatory medications to reduce the swelling in the bursa, advice on different footwear, prescribe a custom made orthotic to try and control the excess pressures through the foot. Ultrasound will help relieve the pain and strapping or padding can reduce the high pressure over a bursitis. Our patients respond to these conservative measures once the area of irritation is removed.
Pain in a child’s foot or ankle is never normal.
There is no such thing as continued common “growing pains.”
Any pain that lasts more than a few days, or that is severe enough to limit the child’s walking should be assessed by the team at Complete Foot Care at the Balcombe Foot and Ankle Clinic
Does your child suffer with any of these?
A Flatfoot – Some children with flat feet have no symptoms.
However they may have trouble participating in physical activities or sports, or appear to walk or run awkwardly.
Some children complain of pain or cramping in their feet, legs or knees.
Any pain or difficulty with a child’s feet should be evaluated by Anna Balcombe specialist in Paediatric Biomechanics.
In toeing – some children walk with their forefoot in turned which can make their gait unstable and clumsy. Many grow out of this by the age of 3or 4 however others may require corrective insoles to help their foot function and prevent future changes and pain in their feet. If you are at all concerned you contact us for advice on Complete Foot Care at the Balcombe Foot and Ankle Clinic.
Heel pain (Sever’s Disease) – Is your child suffering with a painful heel—this maybe due to inflammation of the heel bone growth plate?
It typically affects children between the ages of 8 and 14 years old, because the heel bone is not fully developed until at least age 14. Until then, any new bone forming at the growth plate maybe under too much repetitive stress and inflammation can develop.
Ingrown Toenails – There are many causes to in growing nails in children including incorrect nail trimming, nail picking, adolescence foot sweating, big toe position and shoes. When the nail breaks the skin, serious infections can result. Never try to dig the nail out at home; always seek help and treatment at The Balcombe Foot and Ankle Clinic.
Warts (Verrucae ) – These can develop anywhere on the foot and they are caused by a virus commonly picked up on wet floors ( swimming pools, shower rooms etc) Typically they appear on the bottom of the foot but can occur anywhere and may grow deep into the skin causing walking or standing painful.
Does your Child have a foot related Problem?
Foot and ankle problems in children often go unnoticed. Signs and symptoms can be subtle, and sometimes children can’t explain what’s wrong. But it’s important to protect growing feet and have problems checked out early by us who will give you Complete Foot Care at the Balcombe Foot and Ankle Clinic.
Here Are Five Signs to Look Out For:
- Your Kids Can’t Keep Up with Their Peers
If children lag behind in sports or backyard play, it may be because their feet or legs are tired. Tiredness, aching legs and an unwillingness to walk are common when children have flat feet. The muscles in the feet and legs tire easily because the feet are not functioning as well as they should. - Children Voluntarily Withdraw from Activities they usually Enjoy
If they are reluctant to participate, it may be due to heel pain — a problem often seen in children between the ages of 8 and 14. Repetitive stress from sports may cause muscle strain and inflammation at the growing plate of the heel bone, a weak area at the back of a child’s heel. - They Don’t Want to Show You Their Feet
Children may feel pain or notice a change in the appearance of their feet or nails but don’t tell their parents. At The Balcombe Foot and Ankle Clinic we encourage parents to make a habit of inspecting their child’s feet starting at a young age. Look for any changes such as calluses, growths, skin discoloration, or redness and swelling around the toenails. These are all sign that you may require a professional Podiatric opinion. - Your Child Often Trips and Falls
Repeated clumsiness may be a sign of in-toeing, balance problems or neuromuscular conditions. - The Child Complains of Pain
It is never normal for a child to have foot pain. Injuries may seem minor, but if pain or swelling last more than a few days, have your child’s foot examined by u for a complete diagnosis with care and treatments for your child.

Corns and calluses on the feet are thickened areas of skin that can become painful. They are caused by excessive pressure or rubbing (friction) on the skin. At Complete Footcare we can cut away (pare) corns and calluses and can advise on footwear, shoe insoles and padding to prevent recurrences.
What are corns and calluses?
A corn is a small area of skin which has become thickened due to pressure on it. A corn is roughly round in shape. Corns press into the deeper layers of skin and can be painful.
- Hard corns commonly occur on the top of the smaller toes or on the outer side of the little toe, often areas where shoes tend to rub most.
- Soft corns sometimes form in between the toes, most commonly between the fourth and fifth toes. These are softer because the perspiration between the toes keeps them moist.
If you develop a painful corn or callus it is best to get expert advice from Complete Footcare at The Balcombe Foot and Ankle Clinic to diagnose and treat foot disorders You should not cut corns yourself.
Advice and treatments usually considered include the following:
The thickened skin of a corn or callus can be pared down and the pain is usually much reduced as the pressure on the underlying tissues is eased. Sometimes, repeated or regular trimming sessions are needed.
Heel fissures, also known as cracked heels can be a simple cosmetic problem and a nuisance, but can also be painful. Heel fissures occur when the skin on the bottom, outer edge of the heel becomes hard, dry and flaky, sometimes causing deep fissures that may bleed.
Why do I suffer from Heel Fissures?
Heel fissures can affect anyone. Factors that worsen the problem are: Living in a dry climate ,obesity, consistently walking barefoot or wearing sandals or open-backed shoes, .If heel fissures go untreated they can become deep or infected, this is especially dangerous for people with diabetes or compromised immune systems.
How Do I Treat / Prevent Cracked Heels ?
Moisturizing the feet regularly can prevent heel fissures. Once they occur, you can use a pumice stone daily to gently decrease the thick and flaky layer of skin. Avoid going barefoot or wearing open-backed shoes, sandals or shoes with thin soles. Shoes with strong shock absorption can help to improve the condition. Moisturizing the feet at least twice a day and wearing socks over moisturizer while sleeping can also help.
It’s especially important to look after your feet if you have diabetes.
How do I take care of my feet if I have diabetes and when should I seek professional help?
Diabetes can reduce the blood supply to your feet and cause a loss of feeling in your feet where they become numb and tingle (pins and needles). This can mean foot injuries do not heal well, and you may not notice if your foot is sore or injured.
- See a podiatrist at least once a year.
- Keep your feet clean and free from infection.
- Wear shoes that fit well and don’t squeeze or rub. Ill-fitting shoes can cause corns and calluses, ulcers and nail problems.
- Never walk barefoot, especially in the garden or on the beach on holidays and try to avoid sitting with your legs crossed.
- Get corns or hard skin treated by a podiatrist.
- Seek treatment from your GP or podiatrist if foot blisters or injuries do not heal quickly.
- Treat ulcers urgently, within 24 hours, especially if there is redness or swelling around the area.
- Stop smoking to protect your feet. If you have diabetes, it’s important to try to stop smoking. Smoking impairs the blood circulation, particularly in people with diabetes.
When should I see a Podiatrist or GP?
- you notice breaks in the skin of your foot, or discharge
- the skin over part or all of the foot changes colour and becomes more red, blue, pale or dark
- you notice extra swelling in your feet where there was a blister or injury
- you have any cause for concern
- At least once a year for a diabetic foot check.
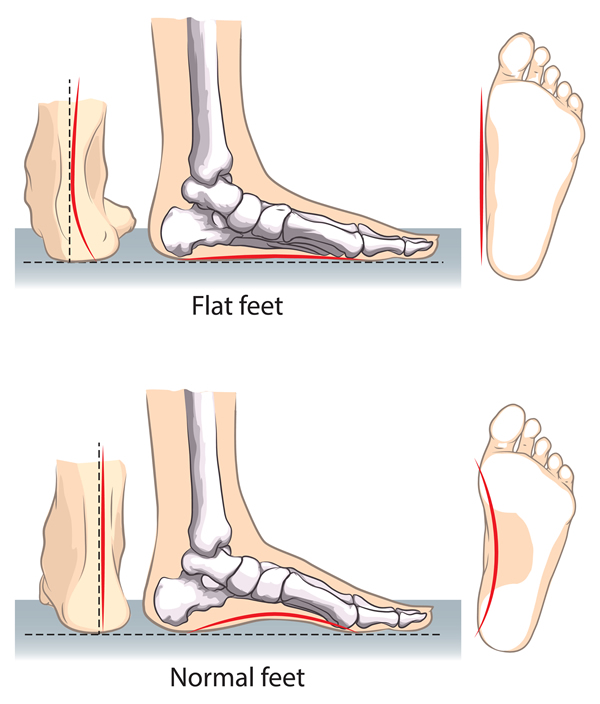
What are Flat Feet?
Flat feet or flat foot is a result of a collapse of the arch of the foot causing your entire foot to lay flat when standing. In some cases this can cause problems with the alignment of your feet, ankles and legs when it forces them to turn inward. This can reduce mobility and sporting activity
What are the causes of Flat Feet?
Many times flat foot or flat feet is caused when the arches of the foot don’t develop properly from childhood. In other cases, flat feet or flat foot can be caused by the arch falling over time due to age or overuse of your foot and ankle. Conditions such as arthritis can cause a flat foot.
What are the Symptoms of a Flat Foot?
Some people experience no signs or symptoms from flat foot while others may have:
- Foot pain in the arch and or ankle
- Difficulty standing on tip toe
- Swelling and discomfort or pain either side of the foot and ankle.
Should I treat a Flat foot?
It is always useful to seek a Podiatrist opinion. Visit us for Complete Foot Care advice at the Balcombe Foot and Ankle Clinic .Treatment of flat feet may include prescription orthotic insoles, footwear advice, physical therapies plus stretching and exercises.
Anna Balcombe, sports Podiatrist can provide an athlete with the tools needed to quickly return to sport after a lower limb injury.

What is Sports Podiatry?
Sports podiatry is the treatment of foot, ankle, knee and leg injuries by altering lower limb function using a variety of methods, including orthotic insoles, footwear and exercises.
One of the most common injuries to affect an athlete is a sprained ankle. Poor biomechanics can cause many types of injuries to the knee. Although sports podiatrists are foot and ankle specialists, correction of foot and ankle mechanics can have a direct influence on knee problems, shin splints, ITB strain, calf or hamstring injury. At The Balcombe Foot and Ankle Clinic we are able to treat these injuries to get you back to your chosen sport as quickly as possible.
What are the common toe injuries that cause forefoot pain?
Sesamoditis
A common injury that affects the big toe, where pain is felt under the ball of the toeon weight bearing and increased levels of activity. Sesamoiditis is caused by poor biomechanics and high impact forces and poor shock absorption in the forefoot.
There are various ways to treat the problem that include patient advice, short term treatment plans including stretching, pain relief and orthotic therapy.
Turf toe – what is it?
More common in sports that involve kicking a ball such as rugby or football. Impaction form kicking causes swelling and pain around the big toe joint and can lead to severe pain.
Hallux Limitus
Do you have a pain in the great toe when standing, running or walking uphill?
Pain is caused by a reduction of movement in the big toe joint, resulting in long term arthritis, pain and mal function. Anna Balcombe, biomechanics specialist will examine the underlying cause of the problem and provide you with a comprehensive treatment plan to return you to pain free walking.
Have I got an Ingrowing nail?
Ingrown toenails occur when the nail grows into the skin at the side of the nail. It is especially common in the big toe and it can be a very painful condition. Starting out as slight redness on the side of the nail but this can quickly deteriorate giving an inflamed red toe which becomes easily infected and produces pus.
Anna Balcombe Podiatric Surgeon will treat the condition with the minimum amount of pain and discomfort and resolve the problem quickly using a variety of surgical and non surgical treatment options. We will also look at the reasons behind the problem and address them promptly giving advice to prevent reoccurrence.
What are the common forefoot injuries?
Morton’s neuroma: this is a nerve impingement problem that affects the forefoot often causing tingling in the toes.
Inter metatarsal bursitis: Symptoms are similar to Morton’s neuroma. It is caused by a fluid filled sac (bursa) and pushing on the nerve causing pain, tingling and numbness.
Plantar plate tear:Occurs when the ligament connecting the toes ruptures or partially tears. This can be particularly painful.
Stress fracture: usually affects bone in the forefoot. It is caused by high impact stresses, lack of shock absorbency and systemic conditions such as osteoporosis.
Capsulitis: This injury affects the joints of the toes (the metatarsal phalangeal joints) the joint gets swollen and inflamed
Are Fungal infections of nails common?
Yes, the infection causes thickened and unsightly nails which sometimes become painful. Medication often works well to clear the infection, but you need to take medication for several weeks. Antifungal nail paints can also help in the early stages.
Who gets fungal nail infections?
Between 3 and 8 out of 100 people in the UK will have a fungal nail infection at some stage of their lives. the infection is just in one nail, but several may be affected.
At first the infection is usually painless. The nail may look thickened and discoloured (often a green-yellow colour or have white lines across the nail. White or yellow patches may also appear where the nail has come away from the skin under the nail; sometimes the whole nail comes away. The nail may become soft and crumble. If left untreated, the infection may eventually destroy the nail and the nail bed, and may become painful. It is important to treat any signs of infection quickly to prevent it spreading.
Pain is the main symptom and this can occur on the underside of your heel and in the arch of your foot. The pain is often worst when you take your first steps on getting up in the morning, or after long periods of rest where no weight is placed on your foot.
Plantar fasciitis is common; around 1 in 10 people will get plantar fasciitis at some time in their life. It is most common in people between the ages of 40 to 60 years however, it can occur at any age.

What is plantar fasciitis?
Plantar fasciitis means “inflammation of your plantar fascia”. Your plantar fascia is a strong band of tissue (like a ligament) that stretches from your heel to your middle foot bones. It supports the arch of your foot and also acts as a shock-absorber in your foot.
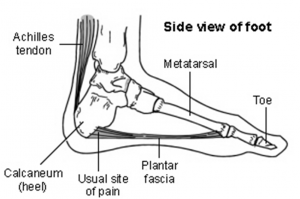
Plantar fasciitis occurs from repeated but small injuries to the fascia (with or without inflammation) are thought to be the cause of plantar fasciitis.
At The Balcombe Foot and Ankle Clinic we specialise in injuries to the foot and we are able to tailor treatment to your specific needs, activity level and footwear.
Treatment varies and can range from reducing the acute pain, addressing the cause of the repetitive strain and inflammation, exercises and stretching advice, physical therapies, heel pads, orthotics to steroid injections and surgical referral if necessary.
What is an Ingrowing toenail?
The nail becomes Ingrowing when the side of the nail cuts into the skin next to the nail. This can become painful. The skin next to the nail may also become infected or inflamed. Any toe can be affected, but it is usually the big toe. It is a common problem, especially in teenagers and young adults.
Ingrowing toenails are treated regularly at The Balcombe Foot and Ankle Clinic both conservatively and in some cases surgery is helpful. Anna Balcombe specializes in foot surgery and has great experience in nail surgery and treatment plus prevention of Ingrowing toenails.
What If the nail fold becomes infected?
Symptoms of infection are: increasing pain, swelling and redness near the Ingrowing nail, and pus (yellow or green fluid) near the nail or under the nearby skin. If the infection is getting worse, you may have a throbbing (pulsating) pain, redness spreading over the toe. You are advised to immerse you toe in warm salt water and seek immediate attention at The Balcombe Foot and Ankle Clinic.
Do you have pain and numbness in your toe?
A neuroma is caused by irritation of a nerve to the toes, most commonly between the second and third or third and forth toes. This condition can be worsened by shoes that squeeze the toes together, thus pinching the nerve between the bones. If a neuroma is present you may experience burning, tingling, cramping or numbness in the forefoot and pain in the tips of your toes.
Through an examination, your podiatrist can determine if symptoms are a neuroma or some other foot problem. Treatment for neuromas may include custom orthotics, footwear advice, ultrasound therapy, medication or surgery.
What to do?
Visit The Balcombe Foot and Ankle Clinic as soon as possible to minimize the likelihood of permanent nerve damage.
Surgery
If conservative care does not help, a surgical procedure can be offered.
Other causes of tingling or “pins and needles” in feet:
- Peripheral neuropathy (nerve damage)
- Nerve entrapment
- Poor blood circulation
- Medication (tingling could be a side effect)
- Systemic diseases, such as hypothyroidism or multiple sclerosis
- Trauma or injury to a nerve, such as with a broken foot
- Vitamin deficiencies
- Alcoholism
- Hormone imbalance
- Infection e.g. shingles
- Autoimmune diseases, such as lupus or rheumatoid arthritis
- Diabetes
- Stroke or seizures
- Raynaud’s phenomenon
- Tarsal tunnel syndrome
Osteoarthritis is also called degenerative joint disease and is the most common types of arthritis .
What are Symptoms and Causes of Osteoarthritis and what joints are affected in the Foot?
Osteoarthritis results in very painful swollen joints and stiffness that occurs with activity. Usually there is no pain before activity or after. As a joints is mobilised you can feel or hear a grinding sound or sensation ( crepitus) .
Causes of osteoarthritis are normally long term trauma by repetitive stresses. This wear and tear may be due to joints not being aligned correctly form birth or from developmental problems like bunion or sudden traumas for example fractured bones.
If the cartilage that covers and protects the end of our bones in the joints is destroyed then osteoarthritis may begin. As the cartilage thins there is narrowing of the joint space and more bone on bone contact causing of pain. The capsule of the joint is affected too.
Areas of the foot that are commonly affected are large toe joints that develop bunions and stiff large toe joints know as Hallux Limitus and Hallux Rigidus. Smaller joints across the top of the mid foot are also affected.
The Balcombe Foot and Ankle Clinic will offer you a diagnosis, advice and various types of treatment to help relieve your pain.
Plantar Fasciitis/ Heel pain
Plantar fasciitis affects the heel and is noted as pain under the heel pad when weight bearing. The symptoms are particularly noticeable when rising from bed in the morning or when sitting for a period of time then standing.
The plantar fascia is a band of tissue, similar to a tendon, which runs from the front of the heel bone to the ball of the foot.
When the foot is on the ground the full weight of the body is concentrated on the plantar fascia and the force stretches the tissue as the arch of the foot tries to flatten from the weight of the body. This in turn leads to stress on the plantar fascia where it attaches to the heel bone, giving rise to small tears of the fascia and pain.
The Balcombe Foot and Ankle Clinic will issue treatment by way of stretches, strapping , advise, heel cushions, ultrasound, hot/cold therapy, orthotics and massage.
Plantar calcaneal bursitis
Symptoms can be very similar to plantar fasciitis, a dull ache under the heel directly under the fat pad.
Tarsal tunnel syndrome
Tarsal Tunnel is a condition that occurs from abnormal pressure on a nerve on the inside of the heel the foot, similar to carpal tunnel syndrome in the wrist.
What is the pain like?
Tarsal tunnel syndrome usually causes a vague pain in the sole of the foot, typically scribed as a burning or tingling sensation which is made worse by activity…. standing and walking for long periods.
How do I treat it?
At our foot and ankle clinic we are able to treat your pain with various pieces of advice, strapping, ultrasound and insoles returning you to pain free activity as soon as possible.
Heel fracture
Fractures are often stress fractures and typically the result of a sudden abrupt injury but can also occur without a history of trauma. Treatment may include the use of X-rays and immobilsatiion followed by rehabilitation.
Pain while running may occur in a variety of signs and symptoms.
Why do I get pain while running?
Poor biomechanics is the single most likely cause of injury. The main biomechanical causes of running injuries are either over pronation or under pronation. These contributory factors are discussed in more detail in our biomechanics section but take a quick look at the videos below to see the biomechanical forces in action in the under and over pronator.
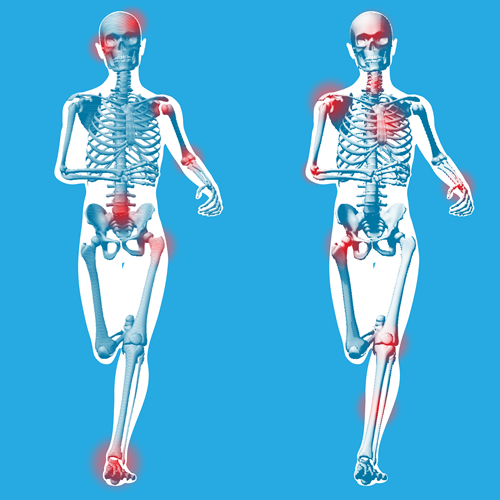
Commom injuries include ;
- Stress fractures – pain under the forefoot
- Sesamoiditis – pain under the great toe
- Ankle strains and sprains (repetitive)
- Achilles tendonitis
- Achilles Bursitis
- Plantar fasciitis – pain in the arch and heel
- Hallux Limitus –pain in the great toe
- Compartment syndrome
- Peroneal tendonitis – pain on the top of the foot extending to the outside of the ankle
- Ankle instability
- Patellofemoral injury at the knee
- Calf strain and the back of the lower leg / knee
- Meniscus tears and co lateral ligament damage at the knee.
- Lower back pain and sacro-iliac inflammation
Running on hard surfaces, over training combined with poor warm up, running shoes that are significantly worn with reduced shock absorption and over tight muscle groups are all factors that contribute to running injuries.
Are your nails causing you a problem ?
Toe nails can be damaged by in a number of ways form repetitive injuries to the toe, such as heavy objects falling on it, pressure from poorly fitting shoes, nail fungus or toe bruising (common in athletes and runners ) .
All of these factors may cause damage to the nail and it`s growth. Sometimes, poor nail cutting may leave a spike of nail that may protrude into the skin as the nail grows outward and if the skin becomes inflamed and swollen due to infection then pain will develop. For an expert opinion, advice and treatment make an appointment with Anna Balcombe.
What Rheumatoid arthritis?
Rheumatoid arthritis is an inflammatory joint destructive disease that cause
Pain and swelling in and around joints commonly effecting women between the ages of 40-60.
Often it involves the toe joints in the forefoot and / or the ankle.
The joints can be very stiff in the morning and usually improve as the day continues. Patients may develop rheumatoid nodules over bony points and symptoms can include as fever, and tiredness.
What Podiatric Care is needed?
Complete Footcare at The Balcombe Foot and Ankle Clinic will aim to increase joint flexibility and muscle strength, and preserve the strength of ligaments and tendons.
Orthotics, custom moulded shoes, or modifications of existing shoes can be used to accommodate foot deformities or rheumatoid nodules and provide relief.
Surgery for patients with rheumatoid arthritis can be helpful to improve the daily living and relief of pressure, Anna Balcombe will happily discuss all foot related treatment options with you.
Verrucae are caused by a virus which produces a wart on the foot.
Are Verrucae painful?
Sometimes they can cause pain to walk on as they increase in size and spread.
They are spread by person-to-person contact or the use of communal showers or wet floors in public swimming areas. They can be treated in a variety of ways including homeopathy, chemical applications, freezing ( cryotherapy) and surgical removal.
Complete Footcare at The Balcombe Foot and Ankle Clinic are happy to discuss your treatment options with you and advise you on the most suitable form of treatment for you.

Products to improve your Foot health
The Balcombe Foot and Ankle clinic stocks a wide range of foot care products to complement care and treatments:
- Curanail £19.50
- Daktarin Cream £4.00
- Krystal Clean Nail £25.00
- Lamisil Spray £6.50
- Lamisil Cream £4.50
- Canestan Cream £4.25
- Lamisil Once £7.50
- CCS Heel Balm £5.50
- CCS Foot Cream £4.50
- Aloe Propolis Cream £11.50
- Warm Your Soles £8.75
- Ditch that Itch £8.75
- Nourish Your Nail £8.75
- Surgical Spirit £2.80
- Thuja 6c £4.50
Plus an assortment of braces, supports, orthotics, therapy and rehabilitation equipment
Orthotics








Biomechanics and Orthotics
Our feet and lower limbs exist to enable us to stand, walk, run, balance and generally mobilise our skeleton. They can change with injury, overuse, sporting activities and age.
They can adjust their structure and shape depending on the task that we are completing.
It is often easier to be mobile rather than standing still on our feet all day as muscular workload is greater when standing still – i.e. foot pressure heightens.
Due to the enormous biomechanical forces we put through our feet, the lower limb, back, and foot are susceptible to complaints and a variety of issues which can be related to misaligned foot and lower limb mechanics.
Gait analysis is used to discover abnormal movements, which can produce high levels of stress in joints and muscles resulting in injury. Orthotics (foot supports) are able to minimize these abnormal movements and stresses.
Complete Foot Care at the Balcombe Foot and Ankle Clinic can help if you have pain in your:
- Achilles tendon
- Ankle
- Ball of the Foot
- Foot arch
- Shins
- Knees
- Back
Our Gait Analysis can detect unusual foot function which may be affecting the rest of your body.
Complete Foot Care at the Balcombe Foot and Ankle Clinic use the latest in 3D optical foot scanners to capture accurate measurements of our patient’s feet. Our scanners are precise at measuring thousands of points around the foot and it`s various contours and with explanation, we are able to show our patients a 3D image of their feet to enable them to understand their own foot mechanics and related pain or problem.
Anna Balcombe has the skill and expertise as a specialist biomechanics practioners to diagnose and use the latest foot scanning techniques to achieve your ultimate orthotic devise.


Orthotics
Orthotics custom made for your specific pain / problem to fit comfortably in your shoes.
Orthotic insoles (foot supports) control the way your foot functions and can compensate for problems and other difficulties in the foot and lower limb, adding support, aiding shock absorption and relieving pain.
At the Balcombe Foot and Ankle Clinic we evaluate requirements based on gait analysis and in conjunction with your personal needs (shoes you wear, your activity level, sporting level.)
We also offer a wide range of “readymade” non bespoke orthotics to suit various foot types and patients needs.
We will recommend the ideal solution for you providing you with advise, exercises and stretching techniques, physical therapies and strapping ankle supports, heel lifts and other devises to reduce your immediate pain and difficulties.
Plus an assortment of braces, supports, orthotics, therapy and rehabilitation equipment








Laser Scanning
We use 3D optical foot scanners that capture accurate measurements of the patient’s feet. These scanners are an extremely precise device measuring thousands of different points of the contours of the foot.
Although 3D lasers are perceived as the latest in technology and one of the most accurate measuring systems for orthotic devices, it is our opinion that no measuring system can surpass the knowledge of an experienced practitioner.
Anna Balcombe has the skill and expertise as a practitioner for your diagnosis, and uses the latest in Laser technology to achieve the ultimate orthotic device.

Address
Complete Footcare at Centennial Medical Care ( CMC ) Unit 509 Centennial Park
Centennial Avenue Elstree WD6 3FG
Complete Foot Care Bodyset 42 Harley St
Marleybone WIG 9PR
Contact
Phone: 07775 995577
Email: annabalcombepodiatrist@gmail.com
More Links
© 2025 Anna Balcombe.

